What is leptospirosis?
Leptospirosis is an infectious disease caused by a bacterium. The bacteria are commonly found in water and soil contaminated with the urine of infected animals. It can present as a mild fever to a severe life-threatening illness.
What causes leptospirosis?
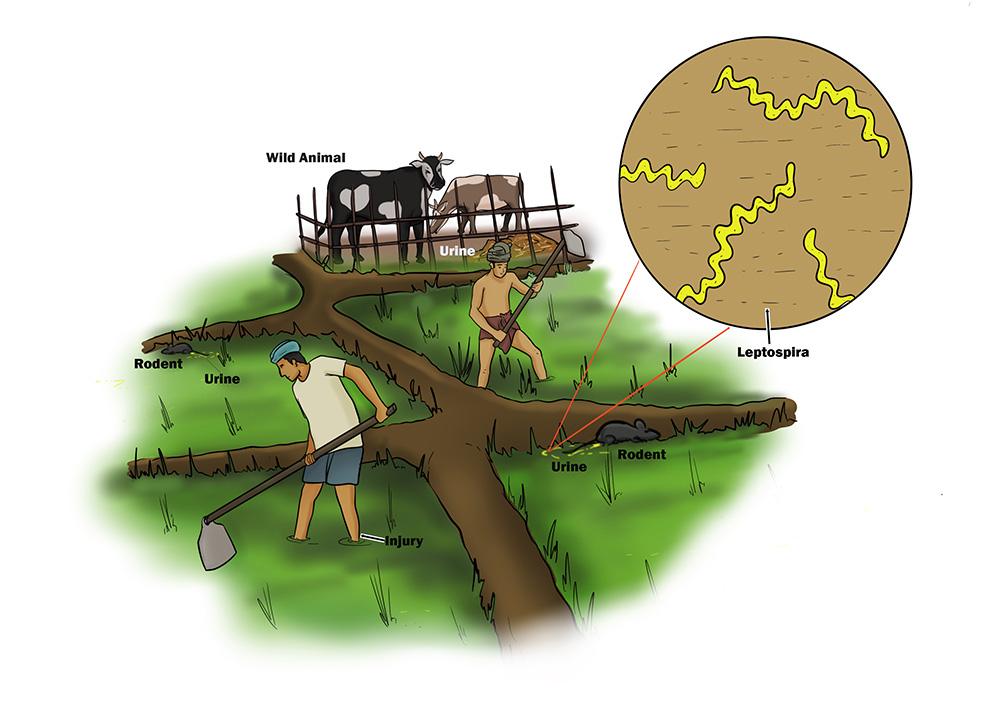
Leptospirosis is caused by various species of Leptospira bacteria. These bacteria are typically transmitted to humans through direct contact with the urine of infected animals, or through water or soil contaminated with the urine. In tropical countries like Sri Lanka, where there is high rainfall, flooding can increase the risk of exposure.
Which animals can spread the disease by acting as carriers?
In Sri Lanka, various animal species can serve as reservoirs for Leptospira bacteria. Common animal reservoirs of leptospirosis include:
- Rodents: Rats and mice are significant carriers of Leptospira bacteria.
- Livestock: Cattle, pigs, and goats can carry and shed Leptospira bacteria in their urine. Farmers and individuals working closely with livestock are at an increased risk of exposure.
- Dogs: Leptospirosis can affect dogs. Therefore, pet owners in close contact with dogs should take precautions to prevent infection.
- Wildlife: Various wild animals, such as deer, raccoons, and small mammals, can carry and transmit the disease. In natural habitats or areas where wildlife interacts with human activities, the risk of exposure may increase.
- Cats: Cats can also carry the disease, though rarely.
What increases the risk of getting leptospirosis?
Exposure to contaminated water with the urine of infected animals increases the risk. The bacteria enter the body by swallowing infected water and splashing contaminated water into the eyes or wounds in the skin.
Farmers, sanitary workers, and veterinarians are the most vulnerable groups. Cleaning drains, gardening, and playing in contaminated water or floodwater increases the risk.
Is it a dangerous illness?
Leptospirosis can range from mild to severe illness. While many cases result in fever-like symptoms that can be managed with proper medical care, severe cases can lead to kidney, lung, heart, and brain involvement and can be fatal. Early detection and treatment significantly improve the chances of a full recovery.
What are the symptoms of leptospirosis?
Leptospirosis may be suspected if you experience symptoms such as:
- High fever with chills
- Headache
- Severe muscle aches
- Yellowish discolouration of the skin and eyes
- Reduced urine output
- Coughing blood
- Difficulty in breathing
If these symptoms occur, especially after exposure to floodwaters, mud, or environments with potential animal urine contamination, leptospirosis is suspected. In Sri Lanka, where the disease is more prevalent, awareness is crucial, particularly during the monsoon season.
What should you do if you develop a fever and suspect leptospirosis?
If you develop a high fever and suspect leptospirosis, seek medical attention promptly. Inform your doctor about any potential exposure to contaminated water or contact with animals. Early diagnosis and appropriate antibiotic treatment are essential to prevent complications.
What should you do to prevent getting infected?
- Avoid Exposure to Contaminated Water: Avoid floodwaters, mud, and stagnant water.
- Use Protective Clothing: Wear boots and gloves if you need to work or be in areas with potential exposure to contaminated environments.
- Practice Good Hygiene: Wash hands thoroughly with soap and water, especially after being in outdoor areas or handling animals.
- Rodent Control: Minimise contact with rodents and practice effective rodent control measures, as they are common carriers of Leptospira bacteria.
- Farmers: You can take a medication (an antibiotic) once a week to reduce the risk of infection. Please contact your MOH office to get the drug during the farming season.
Can the disease spread from one person to another?
Leptospirosis does not commonly spread from one human to another. So, you will not get infected by another infected family member.
Is there a vaccine to prevent the infection?
There is no vaccine to prevent infection in humans yet. Prevention is mainly by avoiding contact with contaminated water.




 info@slcim.com
info@slcim.com